
After a feeding, your baby may need to burp. This small gesture is an essential physiological reflex. Why is burping so important for your infant? What are the best practices to encourage burping after breastfeeding?
Burping your baby after breastfeeding: here’s what you need to know.
Understanding infant burping after breastfeeding
Infant burping is a natural reflex that contributes to your baby’s comfort after feeding. Understanding the role of burping, knowing how to encourage it, and adopting good breastfeeding habits helps soothe your baby and makes feedings more enjoyable for both of you.
Definition and mechanism of burping
During feeding, whether at the breast or with a bottle, your infant swallows not only breast milk or formula but also a small amount of air. This air can build up in the stomach and cause discomfort, or even crying or colic. This is a completely natural physiological phenomenon that often occurs during your baby’s first months of life.
Your baby therefore needs to expel this excess air through a burp. It is important to distinguish burping from regurgitation, which involves the upward flow of a small amount of milk, sometimes mixed with saliva, due to the immaturity of the sphincter between the stomach and the esophagus.
Why is burping important after breastfeeding?
Helping your baby burp after each feeding provides several benefits for digestive comfort:
- Reduced digestive discomfort: releasing swallowed air helps prevent a bloated tummy and colic, and decreases the likelihood that your baby will cry after feeding.
- Prevention of regurgitation: an effective burp after breastfeeding or bottle-feeding reduces pressure in the stomach, lowering the chances of milk flowing back up into the mouth.
- Overall well-being: with less trapped air, your baby is more relaxed, making feedings smoother and creating a calm atmosphere during cuddle time.
How to avoid excessive air intake during feeding?
Burping is not always necessary, especially for breastfed babies whose sucking is often gentler and more effective, reducing air intake. Although the sucking reflex is innate, it may take time to become fully efficient.
For a comfortable and effective feeding session, it is essential that both you and your baby are well positioned:
- Make sure you are comfortable—sit in a chair with armrests, a footrest, or cushions to avoid tension.
- Your baby should be placed in a flexed position. Their neck and pelvis should be supported, their body slightly curled, their feet together and braced, and their hands near their face or your breast. This posture promotes motor stability, allowing for effective sucking and a good latch.
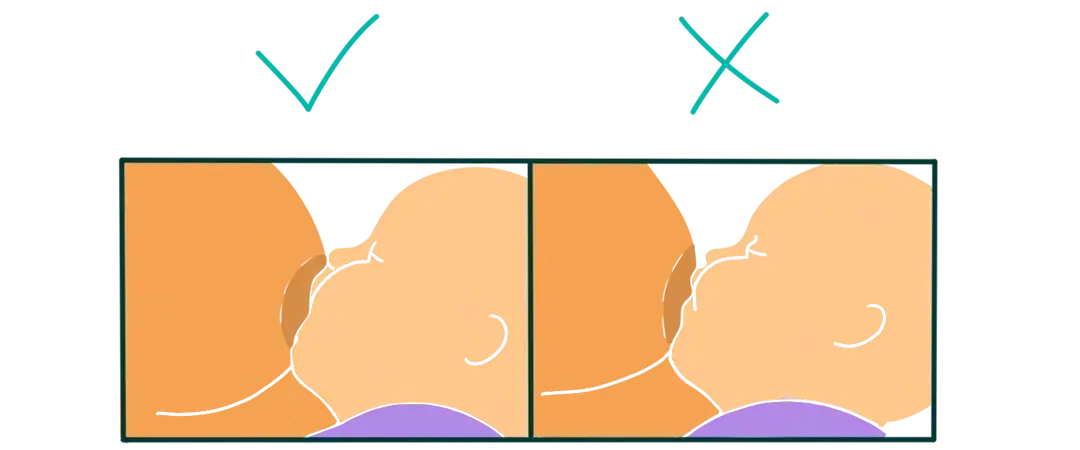
- When latching, your baby’s head should tilt slightly back, with the nose clear and the chin touching your breast. Their mouth should cover a large portion of the areola, creating a seal. If possible, practice skin-to-skin contact, with your baby’s belly against yours and their ears, shoulders, and hips aligned.
Finally, there are many ways to breastfeed. If feeding is not painful and milk transfer is effective, there is no need to change positions. The right position is the one that works for both of you.
Want to learn more? Feel free to download the May app, where you’ll find plenty of resources to support and guide you throughout your journey as a new parent.
Best practices to help your baby burp after breastfeeding
Helping your baby burp after breastfeeding is a simple yet valuable gesture to prevent discomfort, colic, and small regurgitations. Here are proven methods to support this physiological reflex daily, whether your baby is breastfed or bottle-fed.
Recommended burping positions
Some positions make it easier for your infant to expel swallowed air during feedings. Here are the most effective and comfortable ones:
- On your shoulder: hold your baby upright against your shoulder, with their head slightly elevated. Support their back and gently pat or rub between the shoulder blades. This posture encourages air to rise, especially after breastfeeding or bottle-feeding.
- Sitting on your lap: sit your baby on your lap, keeping their torso upright with one hand while supporting their chin (not the throat!). Use your other hand to gently pat their back.
Good to know: Your baby’s position after feeding also matters. Hold your baby upright, in your arms or in a baby carrier, for 20 to 30 minutes after each meal. This encourages natural milk descent and air release, reducing reflux risks and supporting effective burping. After feeding, avoid semi-reclined baby seats and car seats, which compress the infant’s abdomen.
Tips to help your baby burp
A few simple actions can encourage your baby to burp after breastfeeding and improve their comfort:
- Take regular breaks during breastfeeding or bottle-feeding: pause every 5 to 10 minutes to allow your baby to burp, especially if they drink quickly. This helps limit air buildup in the stomach.
- Check the latch and nipple or bottle teat position: a good latch reduces air intake. If your baby seems to swallow a lot of air, adjust their position.
- Avoid tight diapers or clothing: a compressed abdomen can hinder air release and promote reflux.
- Change your baby before feeding: this avoids handling them too much right after a meal, which could trigger regurgitation.
- Adjust the length and frequency of feedings: offer more frequent but smaller feedings or bottles to avoid a gastric “overload,” which can cause reflux and discomfort.
In addition to these tips, closeness, cuddles, skin-to-skin contact, and patience reassure your baby, strengthen your bond, and support calmer digestion—especially during the first months. 
Infant burping: when to worry and consult a healthcare professional
Although burping after feeding is usually natural and physiological, certain signs in your baby may require medical attention.
Unusual symptoms to watch for
While most burps and regurgitations are harmless, some warning signs should prompt you to consult quickly:
- forceful, repeated projectile vomiting,
- the presence of blood or yellow/green bile in regurgitation,
- your baby appears lethargic or excessively sleepy (low energy, difficulty waking),
- a swollen, hard, or painful belly,
- episodes where your baby becomes pale or blue, loses muscle tone, or struggles to breathe during regurgitation,
- persistent, inconsolable crying, especially during or after feedings,
- ongoing digestive issues: diarrhea, recent constipation, reflux appearing after 6 months of age,
- lack of weight gain or stagnant growth despite regular feedings.
Medical follow-up for infants
Your pediatrician supports you throughout the first months to ensure that your baby’s feeding routine is appropriate. During regular check-ups, they:
- Monitor your baby’s weight gain and growth curve.
- Check how feedings are going and assess sucking quality.
- Evaluate the frequency of burping, colic, regurgitations, and crying.
- Provide guidance on breastfeeding practices or bottle preparation.
- Reassure you about common digestive issues or recommend further tests if needed.
This follow-up helps detect any potential concerns early and tailor advice to your situation. Never hesitate to share your observations or concerns. Every baby has their own rhythm.
In summary, ensuring your baby’s digestive comfort involves simple actions. Helping release swallowed air prevents colic, regurgitation, and crying caused by uncomfortable digestion. A good feeding position, proper baby alignment, and gentle handling are often enough to support this process.
Each baby is unique—some need to burp after every feeding, while others need it less often. The most important thing is that your baby is calm, digests well, and gains weight normally. If you notice any unusual symptoms or have concerns, don’t hesitate to speak with a healthcare professional.
**
Photo credits: marne123424 | nd3000
Peux-tu traduire le texte WordPress en anglais US tout en conservant intactes toutes les balises HTML (titres, styles, balises <span>, etc.) ? Je veux uniquement que le contenu textuel soit traduit, sans toucher à la structure HTML. Retire les liens qui commencent par <a href= (sauf s’il s’agit d’une image) mais laisse tout le reste. Envoie-moi l’intégralité de la traduction dans cette conversation, en faisant le moins de messages possible.




