
Breastfeeding is a special bonding moment between a mother and her baby. But sometimes, unexpected issues can arise. Let’s take a closer look at one of them: mastitis.
Here’s everything you need to know!
What is mastitis during breastfeeding?
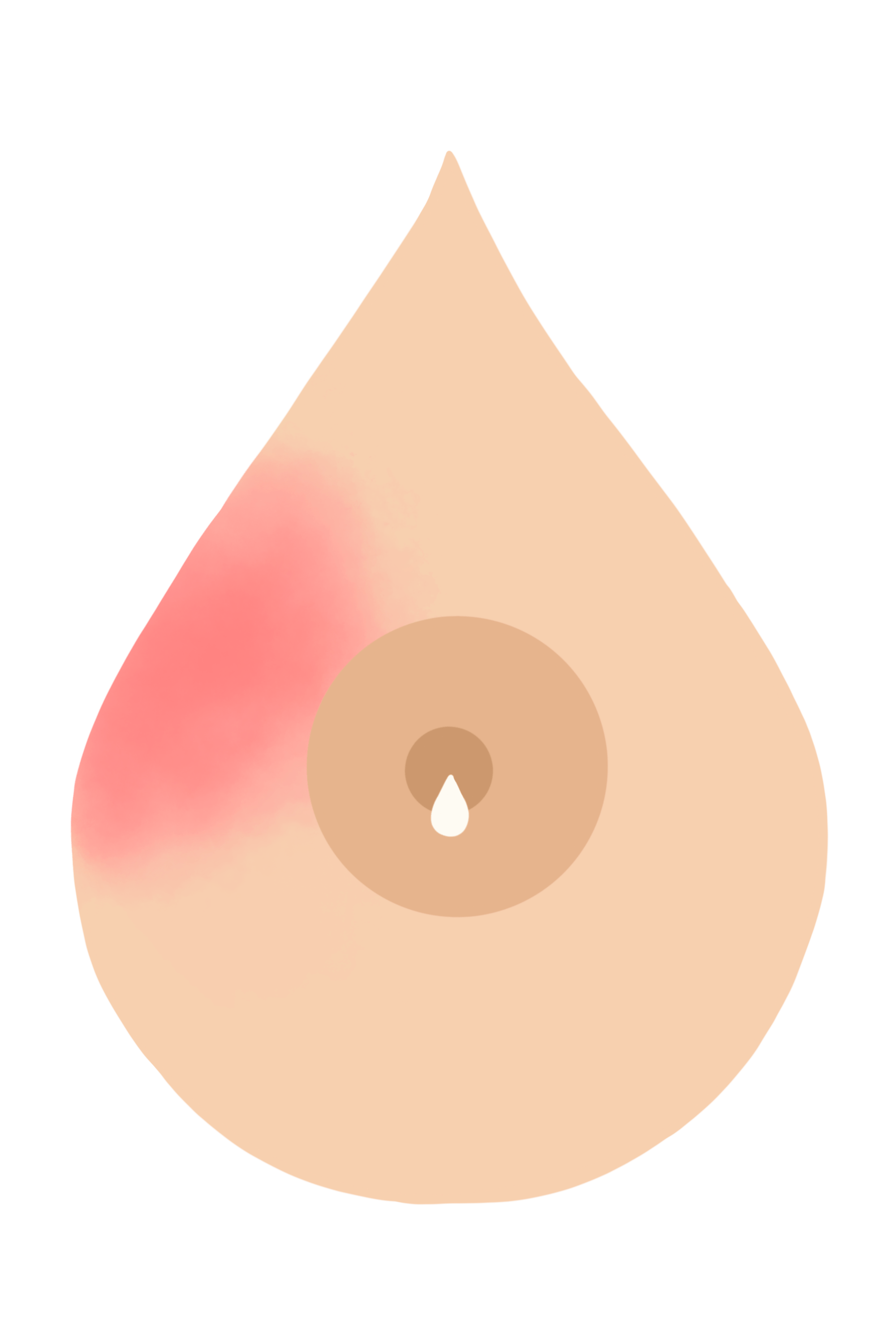
Nearly one in four breastfeeding women will experience one or more episodes of mastitis during their breastfeeding journey. But what is it exactly? Simply put, mastitis is inflammation of a part of the breast and the mammary gland (the part of the breast that produces milk to feed your baby).
When we talk about inflammation, we mean the typical immune system response to external aggression: the skin becomes red, warm to the touch, and even painful.
Mastitis occurs when the breasts become engorged, usually because the baby nurses infrequently or improperly, which can block a milk duct. When a duct is blocked, milk builds up and causes inflammation (mastitis).
Good to remember: it’s important to have a good breastfeeding position. Ensuring proper milk transfer significantly reduces the risk of engorgement.
A good position is first and foremost one in which the mother is comfortably settled, and the baby can open their mouth wide enough to latch onto the nipple as well as part of the areola and breast. This allows them to use their natural skills to feed effectively, drain the breast, and maintain a pain-free milk supply.
In case of pain, we recommend trying the “biological nurturing” position, which puts less strain on the nipple. Your baby lies on you while your torso leans slightly back.
What are the symptoms of mastitis?
Mastitis is sometimes called “breast flu” because the symptoms are quite similar… to the flu. That means: fever, body aches, fatigue, and general malaise.
Mastitis is fairly easy to identify due to its characteristic symptoms:
- It is unilateral (affecting only one breast),
- It is localized,
- The area is red, inflamed, hard, painful, and warm to the touch,
- It is often accompanied by fever (a temperature over 101.3°F / 38.5°C),
- And a flu-like state with chills, aches, fatigue, etc.
Mastitis or engorgement: what’s the difference?
Sometimes, it’s hard to tell at first glance whether it’s mastitis or engorgement. Here are a few tips to help you distinguish between them.
Location: mastitis is always unilateral, whereas engorgement is usually bilateral. It’s rare, but possible, for engorgement to affect only one breast.
Symptoms: mastitis causes flu-like symptoms as well as a red, painful, and localized area on one breast. Engorgement, on the other hand, causes the breasts to feel tight, swollen, sensitive, or painful.
Temperature: mastitis causes fever, while engorgement typically does not or causes only a slight increase in temperature.
How to prevent mastitis while breastfeeding?
We know that certain factors increase the risk of mastitis:
- Cracked or damaged nipples,
- Infrequent feeds, scheduled feeds, and/or timed feeds,
- Skipping a feeding session,
- Poor latch,
- Pressure on the breast (bra, seatbelt, sleeping on your side or stomach, baby carrier…),
- Milk blister (inflammatory lesion on the nipple),
- Stress, fatigue,
- Untreated engorgement.
Some of these factors, like stress and fatigue, are hard to avoid as a parent — we get it. But try to reduce them as much as possible by asking for help from loved ones.
❕Another thing to watch for: weaning. Weaning too quickly can affect your body and lead to engorgement or mastitis. We recommend opting for gradual weaning to allow a smooth transition.
Want to learn more? Feel free to download the May app, where you’ll find plenty of resources to support and guide you throughout your journey as a new parent.
What are the effective treatments for mastitis?
Don’t worry: most treatments for mastitis are easy to implement and generally very effective, not to mention natural. You can:
- Empty your breasts by nursing your baby as often as needed, starting with the unaffected breast,
- Use gentle massage (deep massage, pumping, or vibrations can make it worse),
- Position your baby so their chin is pointing toward the red area,
- Gently massage the breast during feeding,
- Relieve tension in the shower until your breast feels comfortable,
- Apply chilled cabbage leaves, cold compresses (like water-soaked diapers frozen into “ice packs”), or clay poultices,
- Rest and stay hydrated,
- Apply heat before nursing and cold afterward,
- Avoid lactogenic foods or breastfeeding teas,
- Gently massage your breasts before feeding to soften them,
- Take paracetamol to reduce fever if needed.
One of the best remedies for mastitis is spending a day in bed with your baby, offering the breast as often as possible!
❕Mastitis can make breastfeeding painful. The key is to avoid a vicious cycle: the less your baby feeds, the less your breast is drained, and the harder breastfeeding becomes.
If these methods don’t work, if symptoms are too uncomfortable, or if mastitis lasts more than 24 hours: consult a doctor. They may prescribe pain relief or anti-inflammatories.
As always, avoid self-medicating. Talk to a healthcare professional before starting any treatment.
When should you see a doctor for mastitis?
If mastitis doesn’t improve after 24 hours of home care, consult a doctor. They may prescribe anti-inflammatory treatment or even antibiotics if complications arise.
Does mastitis affect the baby’s health?
No, mastitis does not affect your baby’s health. However, the milk may become saltier, and your baby might refuse to nurse from that breast. If that happens, offer the other breast instead.
Since mastitis is not caused by a virus, even though symptoms might suggest it, there’s no risk to your baby.
Does mastitis during breastfeeding mean you need to stop breastfeeding?
Ideally, the answer is no! As we’ve seen, your baby is not at risk. However, pain is one of the leading reasons parents stop breastfeeding in the first few weeks. And yet, mastitis and breastfeeding pain are problems that can often be resolved with the right help.
That’s why it’s so important to get the support you need. Don’t hesitate to reach out to a certified lactation consultant (IBCLC). These health professionals are there to help, answer your questions, and provide guidance.
On May, you can chat with our team of pediatric nurses — some of whom are also certified IBCLCs — 7 days a week from 8 a.m. to 10 p.m.
Mastitis is a common but treatable complication of breastfeeding. It poses no danger to your baby and can be managed! So don’t hesitate to seek support — you deserve it ❤️.
Written by Sonia Monot with May’s medical experts.
–
Photo: StiahailoAnastasiia
This text was translated from French by an artificial intelligence. The information, advice, and sources it contains comply with French standards and may therefore not apply to your situation. Make sure to complement this reading by visiting the May US/UK app and consulting the healthcare professionals who are supporting you.




