
According to the National Institute of Health and Medical Research (Inserm), ectopic pregnancies account for 2% of pregnancies, affecting approximately 15,000 women per year in France. What does this significant yet relatively little-known complication entail? How can it be detected?
Ectopic Pregnancy: Let’s take a closer look.
What is an ectopic pregnancy?
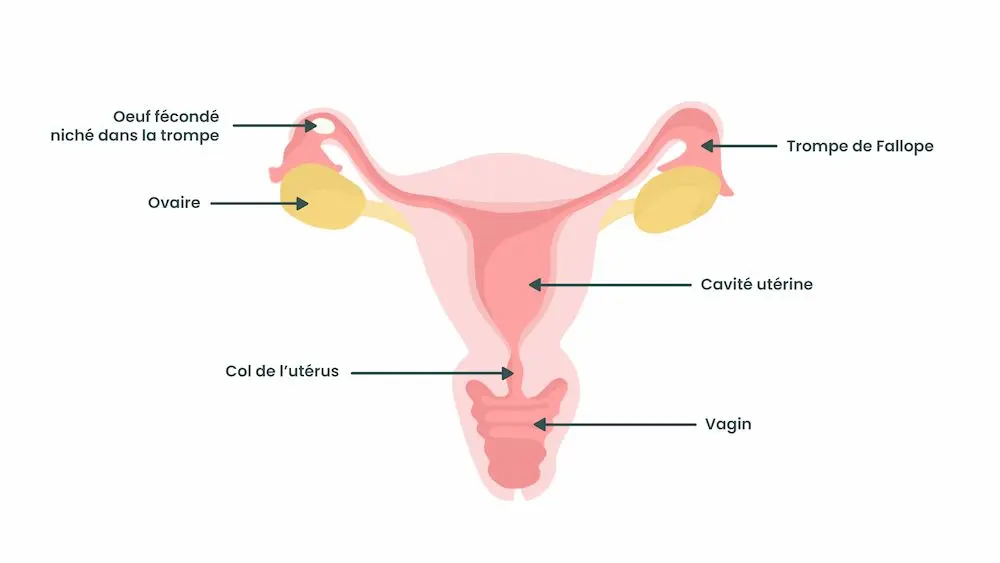
An ectopic pregnancy (EP) is a serious complication of pregnancy. Specifically, during implantation, the fertilized egg implants outside the uterine cavity (unlike a “normal” pregnancy, referred to as an intrauterine pregnancy) and thus outside the endometrium. Typically, the egg implants in one of the two fallopian tubes instead of continuing its journey to the uterus (as it normally should).
Good to know: we refer to it as a pregnancy because fertilization of the ovum by a spermatozoon has occurred; however, this pregnancy cannot proceed. An ectopic pregnancy cannot develop or result in a child at term. It must be terminated, whether spontaneously, medically, or surgically. An EP also poses a danger to the pregnant woman’s health and must be treated promptly.
Risk factors for an ectopic pregnancy
Even though its origin is not always determined, an ectopic pregnancy can be favored by certain factors. The main ones are divided into two broad categories.
History of upper genital infections
Upper genital infections (caused by bacteria such as chlamydia, gonococcus, or mycoplasma) can affect the fallopian tubes, particularly by reducing their mobility. The tube through which the fertilized egg passes will then have more difficulty “pushing” it towards the uterine cavity. The egg is then more likely to implant directly in the tube.
Good to know: yeast infections are not upper but lower genital infections – they do not expose one to this type of risk!
Smoking
You probably already know that smoking is strongly discouraged during pregnancy: the same applies during the preconception period. Indeed, smoking affects the tiny cilia inside the tubes, which help transport the egg to the uterus. For this reason, it is strongly recommended to quit smoking as soon as you have a pregnancy plan.
If you have difficulty overcoming this addiction, do not hesitate to seek help from a healthcare professional, use the toll-free number available on tabac-info-service.fr or download the Tabac info service application.
What other factors?
There are other, less common risk factors, such as a history of surgery on the tubes or the use of in vitro fertilization (IVF).
Also note that the intrauterine device (IUD) protects against intrauterine pregnancies but not against EPs. Therefore, it is possible to have an EP even with an IUD. However, an IUD is not itself a risk factor for ectopic pregnancy.
Finally, be aware that in most cases of ectopic pregnancies, none of the previously mentioned risk factors are observed.

How to recognize an ectopic pregnancy: what are the symptoms?
How to identify an ectopic pregnancy? Does it cause specific symptoms?
Symptoms of EP
The symptoms of an ectopic pregnancy can be particularly difficult to establish as they are often identical to the signs of early pregnancy. Sometimes, an EP is completely asymptomatic.
Nevertheless, one may observe randomly and depending on the woman:
- abdominal pain that can be either diffuse throughout the lower abdomen or localized (lower right or lower left),
- bleeding, which can be brown or blackish. The amount varies among women.
Good to know: any bleeding during pregnancy is not necessarily indicative of an EP; however, they should automatically lead to a medical consultation to ensure everything is fine.
Also note that an ectopic pregnancy can lead to a major complication: rupture of the tube. This is an internal hemorrhage, manifested by a fainting spell (with or without loss of consciousness), severe abdominal pain, vomiting, radiating shoulder pain… If you notice these symptoms, go immediately to the gynecological emergency room; it is a life-threatening emergency.
How to distinguish an EP from another pathology?
Due to its symptoms, sometimes difficult to identify, it may be challenging to distinguish an EP from another pregnancy complication such as miscarriage (now more commonly referred to as pregnancy loss). Here are the main differences:
| Criteria | Ectopic Pregnancy | Miscarriage |
| Definition | Implantation of the embryo outside the uterus (often in the Fallopian tube). | Spontaneous interruption of the pregnancy. |
| Location of the egg | Outside the uterus (Fallopian tubes, ovaries, abdomen). | Inside the uterus. |
| Symptoms | Severe and localized pelvic pain, irregular vaginal bleeding, sometimes fainting or shoulder pain (in case of rupture). | Heavy vaginal bleeding, abdominal pain similar to menstrual cramps, disappearance of pregnancy symptoms. |
| Progression | May lead to rupture of the tubes, internal bleeding, and hemorrhagic shock if left untreated. | Spontaneous expulsion of the embryo or need for medical management (medication or suction). |
| Prognosis | The pregnancy cannot continue and may affect fertility if the tubes are damaged. | The pregnancy cannot continue either but the prognosis is generally good, with the possibility of conceiving again without major complications. |

Diagnosing an Ectopic Pregnancy
To confirm an ectopic pregnancy, your healthcare professionals need to verify the presence of the fertilized egg outside the uterus (as we’ve seen, most often in the fallopian tubes).
To do this, an ultrasound scan is performed: the diagnosis is not always straightforward because the ultrasound image is a reconstructed image made with sound waves—it is not a photograph or a video. As a result, doctors often speak of a suspected ectopic pregnancy—without full certainty. Three scenarios are possible following the ultrasound:
- Pregnancy is seen in the tube: the diagnosis of ectopic pregnancy is confirmed. For this, the gestational sac must be large enough to be visible on the ultrasound. This is referred to as a lateral uterine mass (a medical term for a pregnancy developing in the tube).
- Pregnancy is seen in the uterus: the diagnosis of ectopic pregnancy is ruled out when the ultrasound shows the presence of a gestational sac with a yolk sac inside (a small white circle that will become the embryo) in the uterus. This is the only way to exclude an ectopic pregnancy.
- The location of the pregnancy is not yet visible on ultrasound: don’t panic! If there are no signs of ectopic pregnancy or intrauterine pregnancy but beta-hCG levels are positive, the pregnancy is called a pregnancy of unknown location (PUL). If there are no alarming clinical signs, the patient will be monitored every 48 hours with hormone level checks.
In cases of ectopic pregnancy, beta-hCG levels (a hormone secreted only during pregnancy) tend to rise very slowly or stagnate instead of gradually increasing (they normally double every 48 hours in a typical pregnancy). For reliable results, beta-hCG levels should always be tested in the same laboratory.
Good to know: for women with a history of ectopic pregnancy, an early ultrasound is recommended (around 6–7 weeks of amenorrhea) to check the location of the pregnancy.
Want to learn more? Feel free to download the May app, where you’ll find plenty of resources to support and guide you throughout your pregnancy.

What to Do in Case of an Ectopic Pregnancy?
You’ve been diagnosed with an ectopic pregnancy? Here are the options your healthcare professionals may offer you.
Is It Possible to Carry an Ectopic Pregnancy to Term?
An ectopic pregnancy cannot and should not be carried to term because it poses a danger to the pregnant woman’s health. Once the diagnosis is made, your medical team will guide you toward the best way to terminate the pregnancy. This may involve medical treatment or surgical intervention (under anesthesia).
Methotrexate Injection
Ectopic pregnancy is a serious complication of pregnancy that requires prompt medical intervention. Although it’s possible for it to resolve on its own, most of the time, medical intervention is still necessary.
If the ectopic pregnancy is located in the tube, your beta-hCG levels are stagnant (or low), and you have no clinical signs of severity (such as feeling faint or severe pain): your healthcare professionals may suggest a methotrexate injection. This is a medication that destroys pregnancy cells from within (therefore, no expulsion of the egg).
Please note that you will be closely monitored in the following days with multiple check-ups to track your beta-hCG levels (which should drop significantly after one week) or to detect any signs of complications. Also, the risk of tube rupture is not entirely ruled out until your beta-hCG levels reach zero.
Surgical Interventions
Surgical treatment for an ectopic pregnancy is recommended if:
- you cannot commit to close and regular monitoring in the case of a methotrexate injection,
- your clinical condition is too severe (severe pain or a drop in blood pressure, for example),
- or if the tube has ruptured.
Depending on your case, different options will be offered:
- Laparoscopy: this is the most common surgical procedure for ectopic pregnancy. The surgery is performed using a camera and instruments inserted through 3 or 4 small incisions in the abdomen.
- Salpingectomy: this is much rarer and involves removing the fallopian tube.
- Laparotomy: in even rarer cases, your healthcare professionals may need to perform a full abdominal surgery (similar to a C-section).

Are There Any Consequences for Future Fertility?
In most cases, fertility is not affected after an ectopic pregnancy. However, the risk of having another ectopic pregnancy is higher in women with a history of ectopic pregnancy. Therefore, stay alert to signals from your body, and if in doubt or concerned, consult a healthcare professional (midwife, gynecologist, etc.). Don’t hesitate to seek support during a future pregnancy plan.
An ectopic pregnancy is therefore a serious complicationthat is not viable and cannot continue. It requires emergency medical intervention. It’s essential to consult a healthcare professional quickly as soon as you notice one or more suspicious symptoms because your health is at stake!

**
Photo credits: simonapilolla | voronaman111 | YuriArcursPeopleimages | zamrznutitonovi | koldunov
This text was translated from French by an artificial intelligence. The information, advice, and sources it contains comply with French standards and may therefore not apply to your situation. Make sure to complement this reading by visiting the May ES/UK app and consulting the healthcare professionals who are supporting you.




