During pregnancy, the baby is inside the uterine cavity, which is closed by the cervix itself sealed by the mucus plug that prevents bacteria from entering. During labor, the cervix gradually opens to allow the baby to pass through; this is called cervical dilation. However, some cervixes begin to change long before labor actually begins.
Let’s help you see things clearly!
At what point during pregnancy does the cervix usually start to open?
Normally, the cervix begins to change just before the last month of pregnancy (except in cases of premature contractions, in which case we speak of a risk of premature birth).
During the last month of pregnancy, the cervix may begin to change under the influence of hormones and possible pregnancy contractions. It softens, shortens, and opens slightly (enough to insert one or two fingers).
However, for other women, the cervix will not change at all before labor begins.
Mothers who have already given birth at least once are more likely to have a modified cervix at the end of pregnancy.
As you can see, as with many things related to pregnancy, there is no absolute rule.
It is only in the days (or hours, depending on the case) preceding birth that the cervix opens significantly thanks to contractions: it softens and shortens, finally dilating to about 10 cm on the day of delivery (this is called full dilation).
What are the usual signs that accompany cervical opening?
It is difficult to tell on your own if your cervix is opening, whether during pregnancy or in the first hours of labor, since dilation itself does not cause any particular sensations.
However, since cervical dilation mainly occurs during labor, it is possible to watch out for these labor signs.
Labor is precisely the period that marks the beginning of contractions until the placenta is delivered. It is a physically intense experience for the body that comes with:
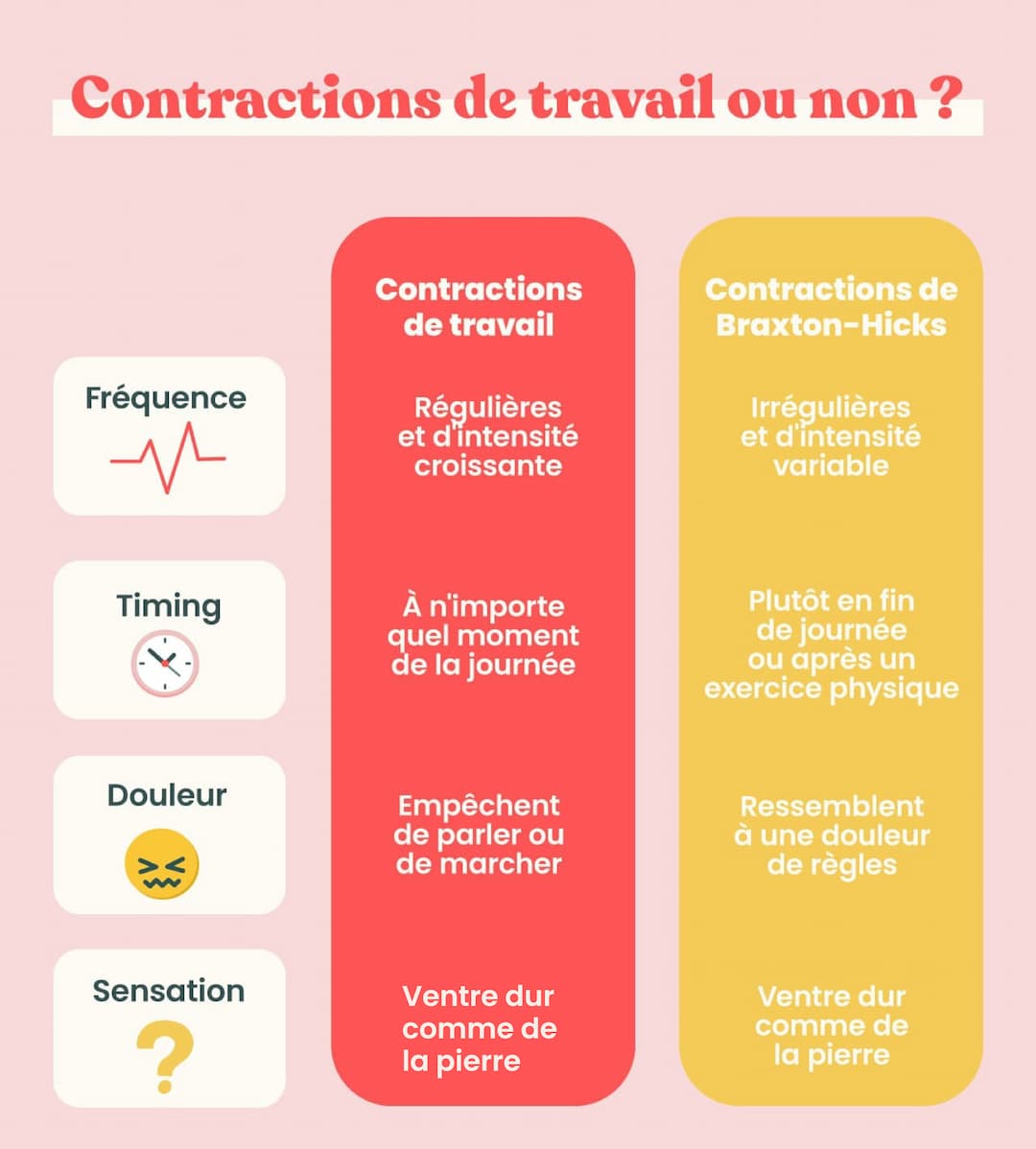
Labor contractions: regular (in frequency, duration, and intensity), becoming closer together and more intense. They encompass the entire abdomen and may radiate into the back. Be careful not to confuse them with Braxton-Hicks contractions (irregular, painless, and resolving on their own). As mentioned earlier, it is the labor contractions that enable the cervix to open.
Rupture of the amniotic sac: either a full rupture (a gush of fluid running down the legs) or a leak (a light flow). When the water breaks before labor, contractions often appear within hours. Why? Amniotic fluid contains prostaglandins—hormones that promote the onset of contractions and cervical changes. Similarly, if the sac ruptures during labor, contractions intensify and cervical dilation becomes easier.
Good to know: losing the mucus plug (a viscous, brownish vaginal discharge) does not predict immediate labor. However, it does indicate that the cervix has probably begun to change slightly (it is not necessary to see a doctor just for this).
Want to learn more? Feel free to download the May app, where you’ll find plenty of resources to support and guide you throughout your pregnancy.
Can I check my own cervical dilation?
In theory, it is possible for a woman to check her own cervical dilation in the same way that healthcare professionals do—by touch, inserting one or more fingers into the vagina depending on the stage. In practice, this is not so easy. During pregnancy, your belly makes the maneuver awkward, if not impossible.
Moreover, very few people can accurately determine whether their cervix is open or not without prior training. This expertise can, for example, be acquired by users of fertility awareness methods (FAM), which are scientific methods for tracking the ovulatory cycle based on daily observation of female fertility “biomarkers.” However, cervical evaluation during labor is quite different, and even with that knowledge, it’s not easy to do.
In any case, it’s best to consult a healthcare professional if you think labor has begun—they can check precisely how dilated your cervix is, if you wish.
What is the importance of cervical dilation in the birth process?
As mentioned earlier, cervical dilation is crucial during childbirth. Thanks to the pressure exerted by the fetal pole on the cervix (the baby and everything around it) with each contraction, the cervix gradually opens. Hormones—prostaglandins and oxytocin—work together to make this possible. As it opens, the cervix creates a passage for the baby to move out of the uterus. This clearly shows the vital importance of cervical dilation.
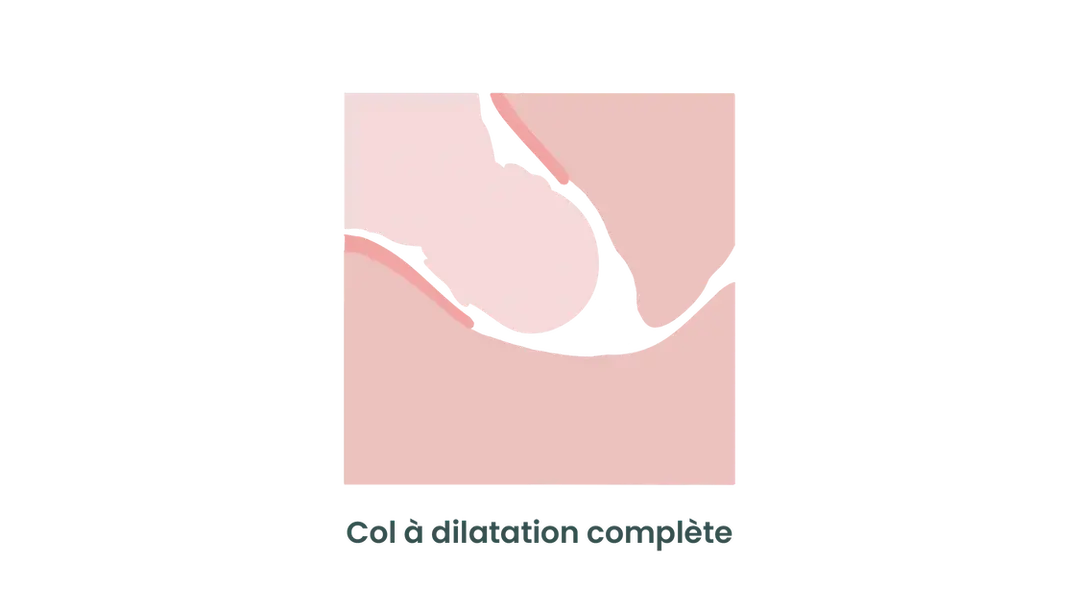
Once dilation reaches 10 cm, the descent and expulsion phase can begin. Conversely, if the cervix stops opening despite active labor, the baby will not be able to pass, which may lead the medical team to perform a cesarean section.
On the other hand, if the cervix opens too early during pregnancy, it may indicate a risk of premature birth. Cervical opening therefore plays a key role in both pregnancy and childbirth.
What are the stages of cervical effacement and dilation?
Cervical dilation and effacement are the first stages of labor, which itself is divided into three stages (dilation, descent, and delivery). It is during the first stage—dilation (itself divided into two phases)—that the cervix changes.
The latent phase
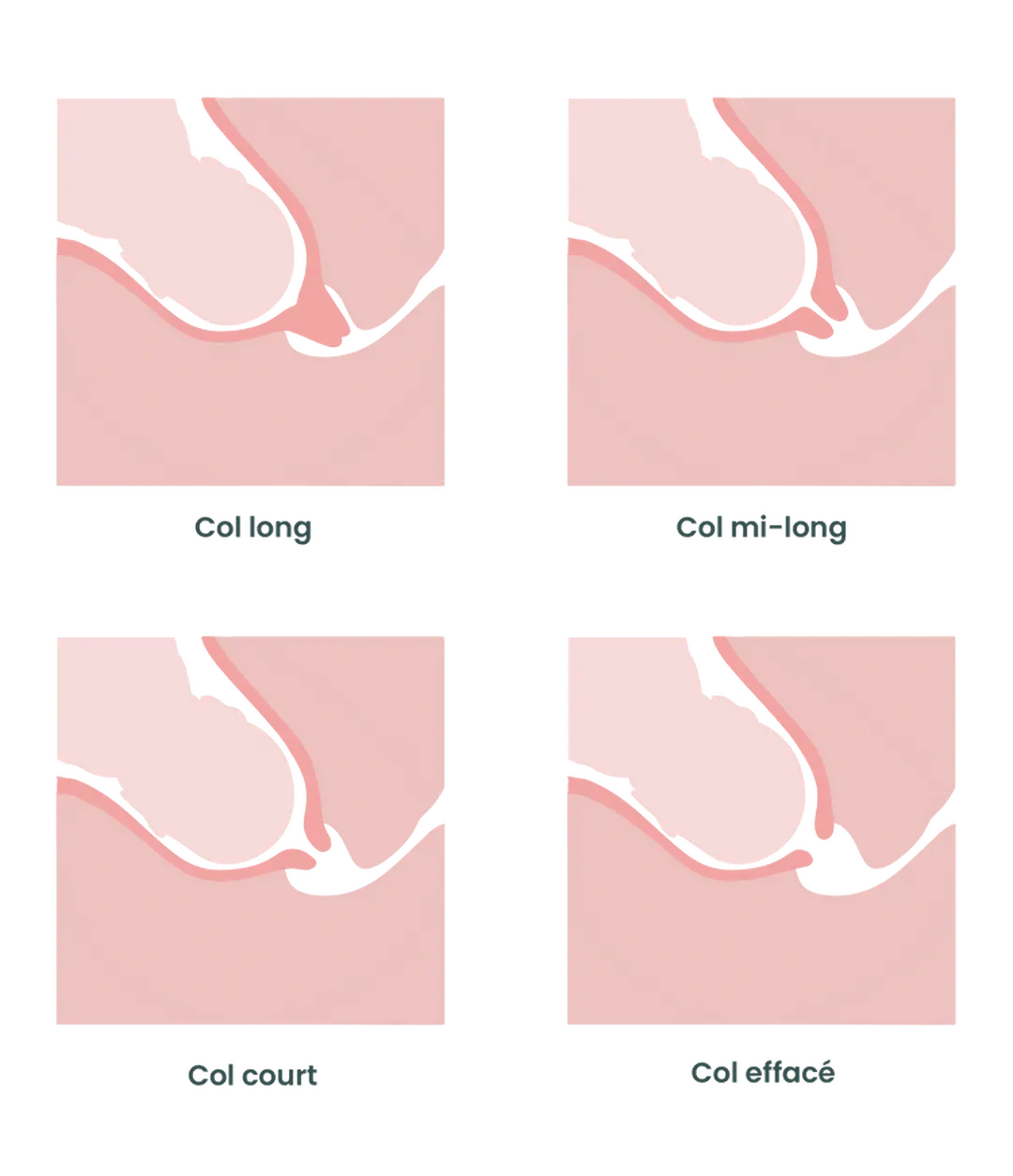
During this phase, which has a very variable duration (from a few hours to several days!), the cervix changes gradually in two main steps: it effaces, meaning it shortens, and then begins to dilate progressively, meaning it opens.
When the cervix effaces during labor, it goes from about 4 cm thick to the thickness of a sheet of paper. It then opens up to about 5 cm (in practice, it often begins to open before being fully effaced).
Other characteristics of the cervix also change during this phase, such as its position and its consistency. The midwife, by performing a vaginal exam, assesses all these factors.
The active phase
During this phase, contractions are very regular and close together and continue to intensify. The cervix keeps opening, moving from 5 to 10 cm of dilation, known as “full dilation.” After a rather slow progression in the previous phase, the rhythm now intensifies sharply.
Once the cervix is fully dilated, the next stages of labor can follow: the baby’s descent into the pelvis, expulsion, and finally delivery of the placenta.
For more information on this topic, feel free to read our article “Labor and Delivery, Step by Step,” written by midwife Anne-Laure Tram on the May app.
Should I see a doctor if I think my cervix is open?
During pregnancy, it’s common to feel a heaviness in the vaginal area: the uterus gets heavier, and its weight can press on the perineum, especially when standing for long periods. This is a common sensation that, without associated contractions, should not be concerning.
As we’ve seen, it’s unlikely that you will actually feel your cervix opening. It’s generally the contractions that accompany this opening that should guide you to the hospital.
➡️ Before 37 weeks of amenorrhea (WA): consult if you have more than 10–15 contractions per day.
➡️ After 37 WA: go directly to the hospital after 1–2 hours of intense, regular contractions (every 5 minutes or less).
Did you know? During childbirth preparation classes, you’ll learn how to recognize labor contractions.
To recap, other reasons to go to the emergency room during pregnancy include:
- Bleeding: regardless of color, amount, or term, any bleeding requires a visit to the maternity emergency room.
- A fall, blow to the abdomen, or accident: your baby is protected by the amniotic sac and uterine wall, but an emergency visit is necessary to ensure the baby’s well-being.
- Fever: if your temperature is above 38°C and you don’t know why, it’s important to consult urgently.
- Your baby is moving less or not at all: if you’re worried because they haven’t moved as usual, eat something sweet and lie down. If your baby doesn’t reassure you within an hour, go to the emergency room for monitoring.
- Rupture of the amniotic sac: always requires an emergency visit—within 1–2 hours if the fluid is clear and you’re not contracting, or immediately if the fluid is green, labor has started, or you’re before 37 WA.
- You feel generally unwell: unusual symptoms (persistent headache, vision or hearing problems, sudden facial swelling, etc.) or any other unusual or concerning signs.
How is cervical dilation assessed during prenatal visits?
Medical check-ups during pregnancy are mandatory (at least one in the first trimester, then at least one per month). They can be carried out by a midwife, general practitioner, or obstetrician-gynecologist.
The healthcare provider will perform a clinical examination (blood pressure measurement, listening to the baby’s heartbeat, measuring fundal height, palpating the abdomen, and others as needed) to make sure everything is going well.
During these appointments, your healthcare provider may also offer to assess (if needed) your cervical dilation using a vaginal examination. However, note that vaginal exams are no longer part of routine check-ups because they don’t provide good predictive value. They are done only at your request or if you have concerning symptoms (always with your consent).
Are there methods to promote healthy cervical dilation?
Sometimes, the cervix can be slow to open. In such cases, you can try adjusting your position during labor to help your baby’s head press more effectively on the cervix. Here are a few examples.
The sitting position
Sit on a birthing ball and lean forward against a wall to stretch your back and relieve your pelvis. You can also lean on the back of a chair while your partner sits on it facing you for support and encouragement.
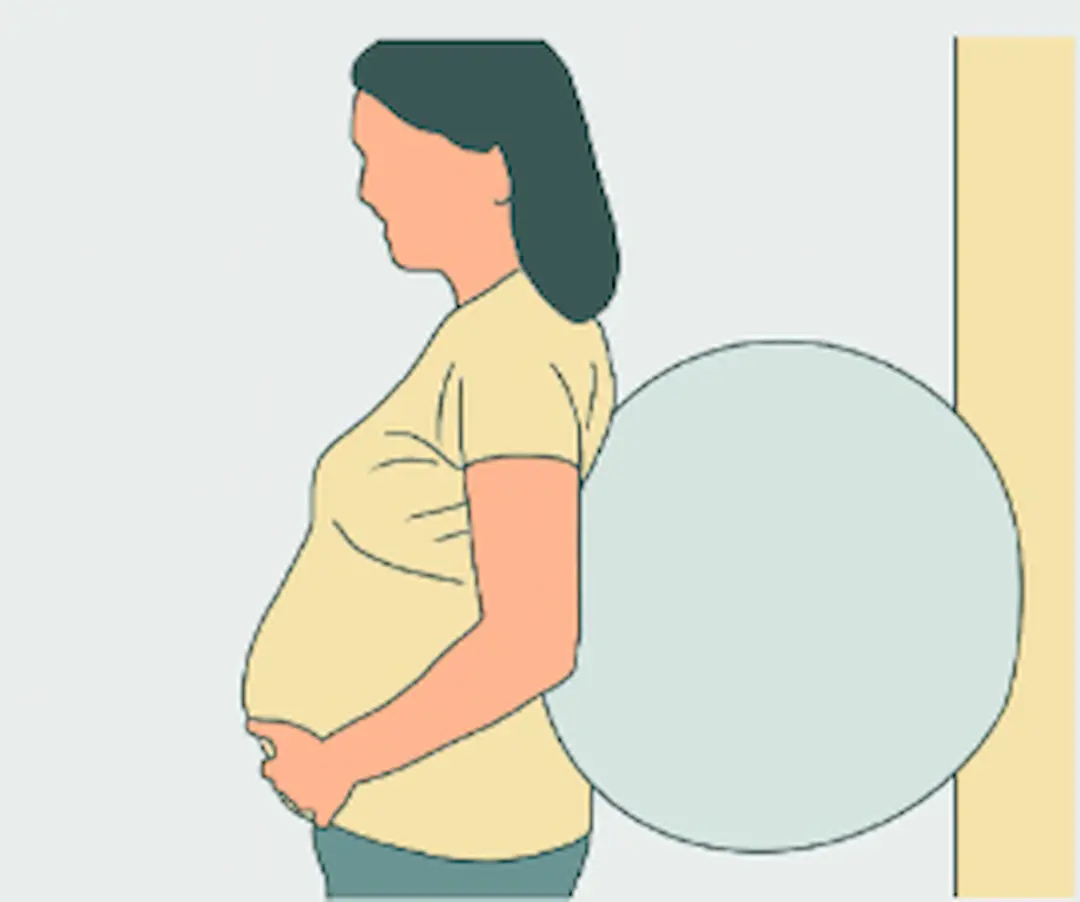
Standing with a ball behind your back
Stand with your legs hip-width apart and slightly bent. Place the ball between your back and the wall. Roll the ball to massage your back.
This position encourages the baby’s descent and can therefore speed up labor. You can also stand against a wall without a ball and sway your hips from side to side for a similar effect.
Psst! On May, we’ve created a practical guide with plenty of other labor positions just for you.
If the dilation phase drags on, your medical team may suggest using medications such as an oxytocin drip (to increase the frequency and effectiveness of contractions) or artificial rupture of the amniotic sac to take advantage of its natural effect on contractions and dilation.
If these measures don’t work either, your healthcare professionals may suggest a cesarean section.
Cervical dilation is therefore a key stage during labor. It’s this opening that allows the baby to pass through the birth canal. Descent can only begin once the cervix is fully dilated to 10 cm.
Don’t hesitate to go to the maternity emergency room as soon as you feel regular contractions, as they mark the start of labor and the end of these nine months of waiting.
Photo: YuriArcursPeopleimages
This text was translated from French by an artificial intelligence. The information, advice, and sources it contains comply with French standards and may therefore not apply to your situation. Make sure to complement this reading by visiting the May US/UK app and consulting the healthcare professionals who are supporting you.