
Among the possible postpartum complications, postpartum eclampsia holds a particular place due to its potential severity. What are preeclampsia and postpartum eclampsia? What are the risk factors? What are the complications?
Postpartum eclampsia: here’s what you need to know.
What are preeclampsia and postpartum eclampsia?
Preeclampsia and postpartum eclampsia are complications related to high blood pressure during and after pregnancy. Here are their symptoms.
Preeclampsia
Preeclampsia is a pregnancy-related condition because it results from an abnormality in placental implantation. It is characterized by high blood pressure associated with dysfunction of certain organs after 20 weeks of amenorrhea (WA). The diagnosis of preeclampsia is made by a doctor or midwife based on data from blood tests and a urine test (to check for proteinuria, meaning the presence of protein in the urine). It most often occurs toward the end of pregnancy. The goal is to detect the condition early in order to limit any maternal or fetal complications.
In France, according to the national health insurance system, preeclampsia affects about 2% of pregnancies and is observed in 70% of cases during a first pregnancy. Among these cases, nearly 10% progress to a severe form.
Postpartum eclampsia
Untreated preeclampsia can lead to several complications, including the development of eclampsia. Although rare, when it occurs after childbirth, it is referred to as postpartum eclampsia. This condition can develop up to 6 weeks after delivery.
Eclampsia is characterized by generalized seizures that affect the mother’s brain in the context of pregnancy-related hypertension. This explains the constant monitoring of blood pressure in the days following childbirth, especially during the first 72 hours.
Symptoms of postpartum eclampsia and preeclampsia
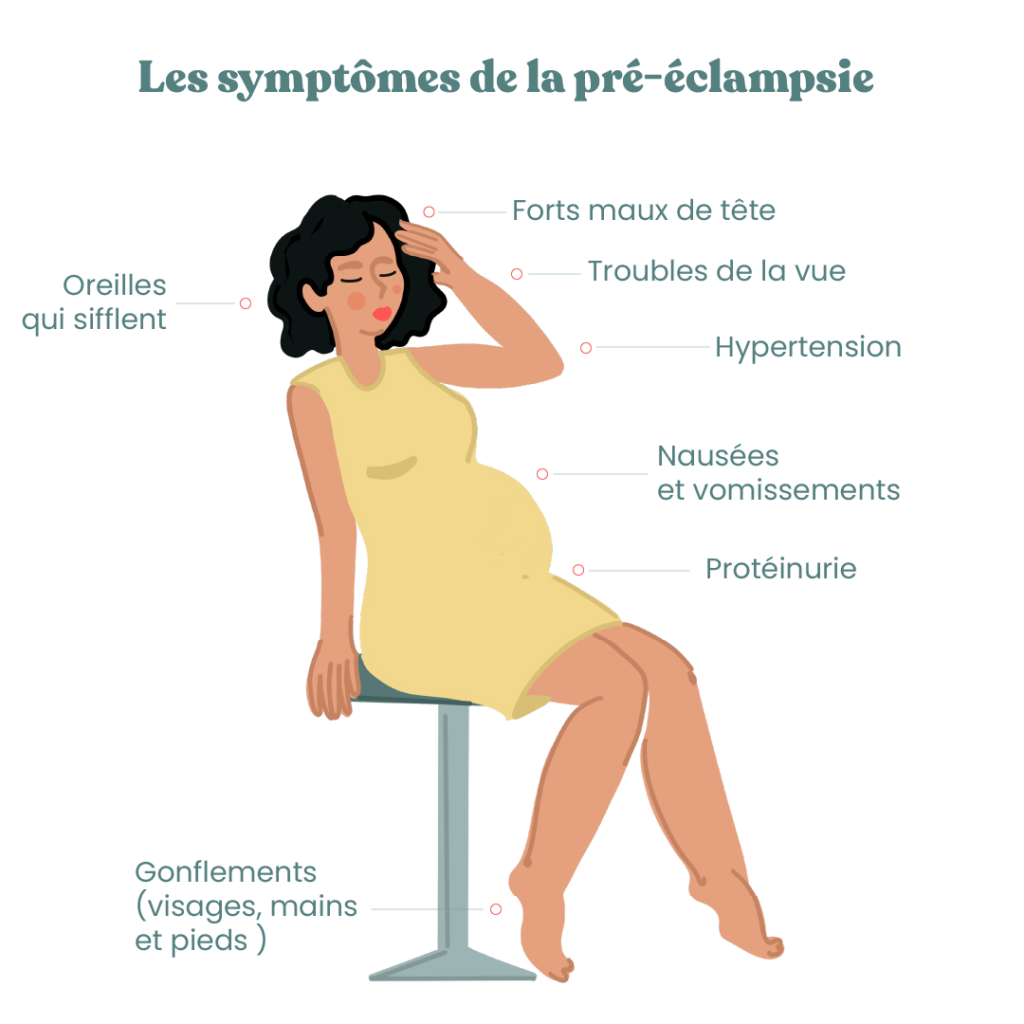
The mechanisms of postpartum preeclampsia are still not well understood since it is a condition linked to the placenta, which normally disappears after childbirth when it is delivered. Beyond high blood pressure, the most common symptoms of preeclampsia are:
- severe headaches,
- ringing in the ears (tinnitus),
- visual disturbances (black spots or “floaters” before the eyes called phosphenes),
- nausea and vomiting,
- swelling, especially of the face or hands (edema),
- a tight band under the chest (intense pain located under the breasts, extending horizontally).
If you experience one or more of these symptoms, it is recommended to promptly consult your healthcare professional. Postpartum eclampsia is a medical emergency requiring immediate hospitalization.
Want to learn more? Feel free to download the May app, where you’ll find plenty of resources to support and guide you throughout your journey as a new parent.
What are the risk factors for preeclampsia?
Some pregnant women are at higher risk of developing preeclampsia. This is particularly the case if:
- You have previously had high blood pressure or eclampsia.
- You have diabetes.
- You are over 40 years old.
- You have obesity with a body mass index (BMI) over 30.
- You are expecting twins (twin pregnancy).
- You conceived through medically assisted reproduction (MAR).
What complications are associated with preeclampsia and how are they treated?
Preeclampsia requires close obstetric management. The major risk following preeclampsia is eclampsia, which is a neurological complication. You will therefore be closely monitored by your medical team. Preeclampsia is problematic because it impairs the circulation of nutrients in the placenta and can cause intrauterine growth restriction.
If the maternity team decides to induce labor before term, medications may be given to the premature baby to stimulate lung maturation, which is still incomplete at that stage (before 34 weeks of amenorrhea).
In the most severe cases, particularly in severe preeclampsia, the mother may suffer a cerebral hemorrhage or even complications affecting the liver, kidneys, and blood clotting. According to several studies, women who experience preeclampsia during pregnancy have a higher risk of developing heart disease later in life.
Preeclampsia is a potentially dangerous condition that requires increased vigilance throughout pregnancy. However, in rare cases, preeclampsia may persist or worsen after birth and lead to postpartum eclampsia, defined by the occurrence of seizures. This is why careful monitoring of blood pressure, during pregnancy as well as after delivery, is essential. If warning symptoms appear, it is important to promptly consult a midwife or physician in order to protect the mother’s health.
**
Photo credits: deriabinanatalia
This text was translated from French by an artificial intelligence. The information, advice, and sources it contains comply with French standards and may therefore not apply to your situation. Make sure to complement this reading by visiting the May US/UK app and consulting the healthcare professionals who are supporting you.




